What is keratoconus?
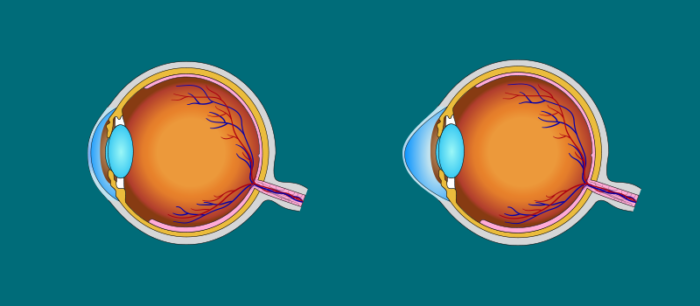
The cornea is the transparent front part of the eye. A healthy cornea is dome-shaped. Keratoconus is a condition which leaves the cornea irregularly convex and thinner. This causes various degrees of sight deterioration, the development of near-sightedness and astigmatism, which cannot be corrected by wearing glasses. In very severe cases, a scar can form at the apex of the cornea.
The condition usually affects both eyes, although it often progresses asymmetrically (i.e. the disease is more advanced in one eye than the other).
Keratoconus is most often diagnosed in adolescents, teenagers and young adults (the average age of diagnosis is 16), far more rarely in people over 30. Discovery may be delayed in less severe cases. It is a progressive condition. The changes may intensify over several years, or more than a decade, and then come to a natural halt at various degrees of progression and damage to the sight.
What are the symptoms?
Unclear vision in one or both eyes, lack of improvement when using corrective glasses, rapid development of sight defects, the need to change glasses frequently, photophobia, problems with driving at night, halo effects.
What are the causes of keratoconus?
The exact causes are not known. It is thought that the disease involves damage to collagen (the material which makes up the cornea), and has a genetic basis. Around 7% of all cases are hereditary. It is often connected with allergies, with atopic inflammation of the skin. There is a clear link between keratoconus and rubbing the eyes.
How can keratoconus be recognised?
During its early and medium stages, the disease can only be diagnosed by visiting an ophthalmologist and carrying out a slit lamp examination and additional tests of the corneal topography and measurement of its thickness.
How is keratoconus treated?
At very early stages of the disease, eyesight can be improved by wearing glasses. At more advanced stages, the right contact lenses must be selected. These are usually small, hard, gas-permeable lenses, although some people may see well using hydrogel lenses or others specially designed for keratoconus. None of these affect the progression of the disease, i.e. they neither intensify nor slow it, they simply improve sight while they are worn.
Cross-linking (CXL) is the latest procedure to treat progressive keratoconus. It consists of applying riboflavin (vitamin B2) to the surface of the cornea, and then irradiating it with ultraviolet radiation of the appropriate wavelength and strength. CXL strengthens the structure of the cornea by increasing the number of cross links between collagen fibres, the material it is made of.
The operation leaves the cornea stiffer, and slows down the progress of the disease. In some cases, a flattening of the conical curve can be observed. Combined treatment can be carried out on certain patients – laser modelling of the corneal surface with CXL.
Intracorneal rings (INTACS) – a pair of arched implants placed in the peripheral part of the cornea in order to flatten out the anterior surface. These are used in cases of intolerance of contact lenses or when they do not help. They enable the cornea transplant to be avoided or postponed.
A cornea transplant may be necessary in cases where the disease is at a highly advanced stage, when there is no possibility to improve the eyesight by any other means, or in conditions when scars form around the cornea.
Prognosis
Most patients achieve an improvement in their sight by wearing glasses or contact lenses. Fewer than 10% require a cornea transplant. A transplant carried out due to keratoconus also has a good prognosis, although the convalescence period may be long, and some patients require contact lenses or refractive laser surgery in the post-operative period.
At Laser CMO, we use the following to treat keratoconus:
- implanting intracorneal rings (INTACS) – we use a femtosecond laser to make the intracorneal canals into which the implants are placed. This means that the operation lasts around 15 minutes and results in the greatest possible improvement in vision.
- “fast cross” KXLAVEDRO – cross-linking using iontophoresis, which dispenses with the need to remove the corneal epithelium before applying the riboflavin in order for it to fully saturate the corneal tissue
- combined technique: laser correction based on corneal topography with cross-linking (EBK+TR+KXLAVEDRO) and INTACS+ KXLAVEDRO
Our staff
Dr. Hab. Justyna Izdebska MD
Graduated from the 1st Medical Faculty of Warsaw Medical University. She has been employed at…show more
Dr. Aneta Bembenek
Eye disease specialist, doctor of aesthetic medicine. Graduated from the 1st Medical Faculty of Warsaw…show more